内分泌干扰物(endocrine disrupting chemicals, EDCs)是一类存在于环境中的天然或人工合成的外源性化学物质,通过干扰激素的合成、运输、转化、结合和代谢等过程来影响生物体的内分泌系统活动。EDCs种类众多、使用广泛[1-5]。一些EDCs属于持久性有机污染物,性质稳定,脂溶性强,进入动物体内容易蓄积在脂肪组织中,很难被分解和排出,其浓度会随着营养级的升高不断增大,导致即便进入环境中的浓度极为微量,也会使生物尤其是处于高营养级生物的内分泌功能受到损伤,特别是在发育易感期[3-4,6]。尽管有些EDCs已被禁止或限制使用,但它们仍然存在于环境中,其环境持久性与生物蓄积性使其暂时或长久地干扰内分泌系统的激素相关信号通路[7],从而影响生长、发育、繁殖、免疫等生理过程,并导致内分泌相关疾病的发生[8-9]。
以哺乳动物细胞、大/小鼠动物模型为试验对象,针对EDCs的毒性效应与机制已开展大量系统研究,但有关EDCs的作用分子靶点的认知仍有待进一步明确。分子结构是决定化合物作用靶点的内因。多数EDCs与天然激素具有结构类似性,可作为配体与激素受体相互作用。本文以雌激素受体(estrogen receptor, ER)、雄激素受体(androgen receptor, AR)和甲状腺激素受体(thyroid hormone receptor, TR)为主,在介绍EDCs对哺乳动物的毒性效应与机制的基础上,聚焦“EDCs干扰激素与受体的结合”这一过程,对近年来EDCs与哺乳动物核受体的相互作用研究进行综述,以期为EDCs暴露的健康风险防范和科学干预提供理论依据。
1 EDCs对哺乳动物的毒性效应与机制(Toxic effects and mechanisms of EDCs on mammals)
EDCs对哺乳动物发挥内分泌干扰作用的主要对象是内分泌系统的下丘脑-垂体-性腺轴(hypothalamus-pituitary-gonad, HPG)(简称生殖轴)和下丘脑-垂体-甲状腺轴(hypothalamus-pituitary-thyroid axis, HPT轴)(简称甲状腺轴)[6-7,10]。在生殖轴中,下丘脑通过分泌促性腺激素释放激素(gonadotropin-releasing hormone, GnRH),调节垂体促黄体生成素(luteinizing hormone, LH)和促卵泡激素(follicle stimulating hormone, FSH)的合成与分泌,它们能够促进性腺合成并释放性激素如雌激素17β-雌二醇(17β-estradiol, E2)、雄激素睾酮(testosterone, T)和双氢睾酮(dihydrotestosterone, DHT)。哺乳动物的生殖主要受到生殖轴的调控[11]。EDCs最早引起科学界甚至公众的关注,也是因为其对生殖轴的干扰作用引起的生殖毒性问题。据此筛选出的最经典的EDCs有双酚类化合物[12-13]、除草剂阿特拉津[14]、有机氯农药滴滴涕[15]、邻苯二甲酸盐及其代谢物[15-16]、多氯联苯[17-19]等。以双酚类化合物为例,围产期暴露于高剂量双酚A,导致其雌性子代成年期发情周期模式发生改变,血浆LH水平降低[12];早期发育(自妊娠第8天至产后第19天)暴露于200 μg· kg-1·d-1双酚S改变了小鼠子宫和卵巢中雌激素反应答基因的表达,并促进雌性后代在出生22 d后卵巢卵泡的发育[13]。
在甲状腺轴中,下丘脑分泌促肾上腺皮质素释放激素(corticotropin releasing hormone, CRH)或促甲状腺激素释放激素(thryotropin releasing hormone, TRH),促进垂体合成和分泌促甲状腺激素(thyroid stimulating hormone, TSH),TSH通过与其特异性受体结合,加速细胞对碘的摄取,进一步促进甲状腺合成和分泌甲状腺激素(thyroid hormones, THs),主要是甲状腺素(tetraiodothyronine, T4),T4在外周组织脱碘转化为活性更高的(triiodothyronine, T3)。EDCs对甲状腺的干扰作用成为研究的新热点[20-27],发现了三丁基锡[21]、双酚A[22]、重金属镉[23]、二乙基羟胺(N,N-diethylhydroxylamine, DEHA)[24]、多溴二苯醚等溴化阻燃剂[25]具有甲状腺干扰作用。然而,由于甲状腺轴在哺乳动物的新陈代谢、能量消耗、生长发育、免疫等多个生理过程中发挥着广泛的调节作用,目前尚不能将EDCs的甲状腺干扰机制与毒性效应建立一一对应关系。
2 EDCs与哺乳动物核受体的相互作用(Interaction of EDCs with mammalian nuclear receptors)
尽管EDCs可以对哺乳动物内分泌系统生殖轴和/或甲状腺轴中一个或多个调控位点进行干扰,影响内源激素的合成、分泌、转化、转运、代谢、结合等过程进而发挥其内分泌干扰效应,干扰激素与受体结合这一过程仍是EDCs发挥内分泌干扰作用的最重要方式,主要有生殖轴的ER、AR和甲状腺轴的TR (表1)。
表1 内分泌干扰物(EDCs)通过受体介导途径发挥内分泌干扰作用
Table 1 Endocrine disrupting chemicals (EDCs) exert endocrine disrupting effects through receptor-mediated pathway
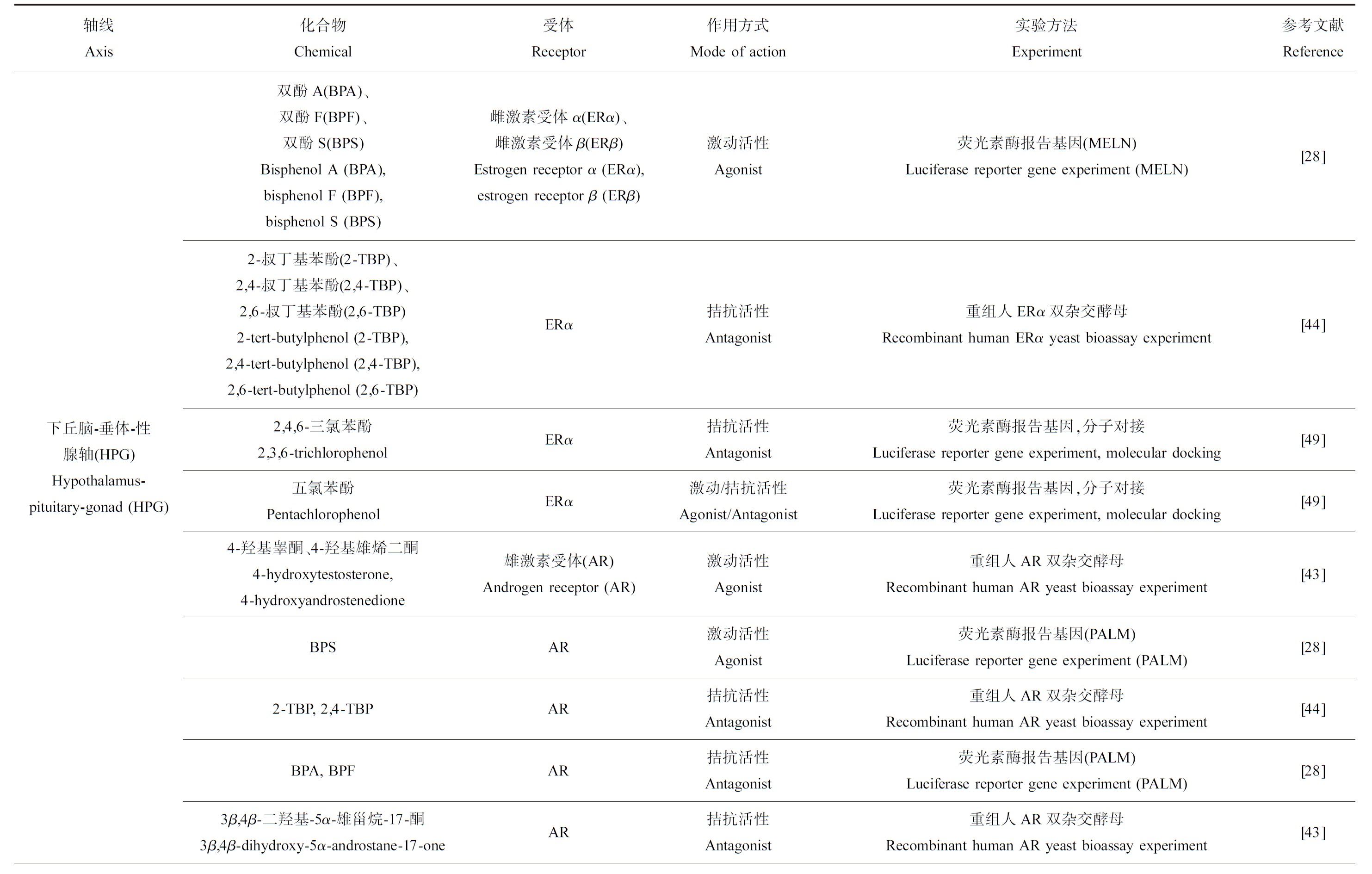
轴线Axis化合物Chemical受体Receptor作用方式Mode of action实验方法Experiment参考文献Reference下丘脑-垂体-性腺轴(HPG) Hypothalamus-pituitary-gonad (HPG)双酚A(BPA)、双酚F(BPF)、双酚S(BPS)Bisphenol A (BPA), bisphenol F (BPF), bisphenol S (BPS)雌激素受体α(ERα)、雌激素受体β(ERβ)Estrogen receptor α (ERα), estrogen receptor β (ERβ)激动活性Agonist荧光素酶报告基因(MELN)Luciferase reporter gene experiment (MELN)[28]2-叔丁基苯酚(2-TBP)、2,4-叔丁基苯酚(2,4-TBP)、2,6-叔丁基苯酚(2,6-TBP)2-tert-butylphenol (2-TBP), 2,4-tert-butylphenol (2,4-TBP), 2,6-tert-butylphenol (2,6-TBP)ERα拮抗活性Antagonist重组人ERα双杂交酵母Recombinant human ERα yeast bioassay experiment[44]2,4,6-三氯苯酚2,3,6-trichlorophenolERα拮抗活性Antagonist荧光素酶报告基因,分子对接Luciferase reporter gene experiment, molecular docking[49]五氯苯酚PentachlorophenolERα激动/拮抗活性Agonist/Antagonist荧光素酶报告基因,分子对接Luciferase reporter gene experiment, molecular docking[49]4-羟基睾酮、4-羟基雄烯二酮4-hydroxytestosterone, 4-hydroxyandrostenedione雄激素受体(AR)Androgen receptor (AR)激动活性Agonist重组人AR双杂交酵母Recombinant human AR yeast bioassay experiment[43]BPSAR激动活性Agonist荧光素酶报告基因(PALM)Luciferase reporter gene experiment (PALM)[28]2-TBP, 2,4-TBPAR拮抗活性Antagonist重组人AR双杂交酵母Recombinant human AR yeast bioassay experiment[44]BPA, BPFAR拮抗活性Antagonist荧光素酶报告基因(PALM)Luciferase reporter gene experiment (PALM)[28]3β,4β-二羟基-5α-雄甾烷-17-酮3β,4β-dihydroxy-5α-androstane-17-oneAR拮抗活性Antagonist重组人AR双杂交酵母Recombinant human AR yeast bioassay experiment[43]
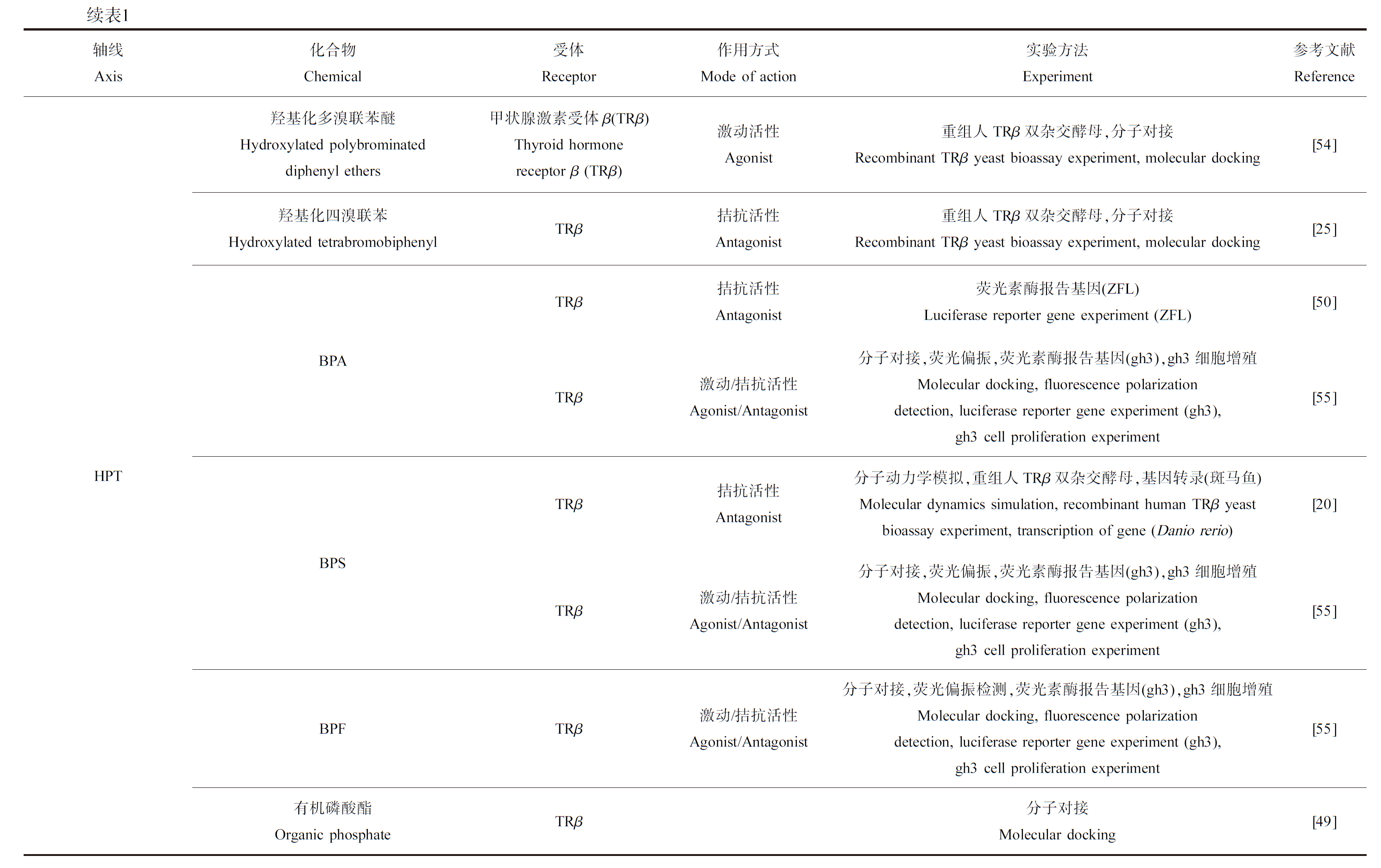
续表1轴线Axis化合物Chemical受体Receptor作用方式Mode of action实验方法Experiment参考文献ReferenceHPT羟基化多溴联苯醚Hydroxylated polybrominated diphenyl ethers羟基化四溴联苯Hydroxylated tetrabromobiphenylBPABPSBPF有机磷酸酯Organic phosphate甲状腺激素受体β(TRβ)Thyroid hormone receptor β (TRβ)激动活性Agonist重组人TRβ双杂交酵母,分子对接Recombinant TRβ yeast bioassay experiment, molecular docking[54]TRβ拮抗活性Antagonist重组人TRβ双杂交酵母,分子对接Recombinant TRβ yeast bioassay experiment, molecular docking[25]TRβ拮抗活性Antagonist荧光素酶报告基因(ZFL)Luciferase reporter gene experiment (ZFL)[50]TRβ激动/拮抗活性Agonist/Antagonist分子对接,荧光偏振,荧光素酶报告基因(gh3),gh3细胞增殖Molecular docking, fluorescence polarization detection, luciferase reporter gene experiment (gh3), gh3 cell proliferation experiment[55]TRβ拮抗活性Antagonist分子动力学模拟,重组人TRβ双杂交酵母,基因转录(斑马鱼)Molecular dynamics simulation, recombinant human TRβ yeast bioassay experiment, transcription of gene (Danio rerio)[20]TRβ激动/拮抗活性Agonist/Antagonist分子对接,荧光偏振,荧光素酶报告基因(gh3),gh3细胞增殖Molecular docking, fluorescence polarization detection, luciferase reporter gene experiment (gh3), gh3 cell proliferation experiment[55]TRβ激动/拮抗活性Agonist/Antagonist分子对接,荧光偏振检测,荧光素酶报告基因(gh3),gh3细胞增殖Molecular docking, fluorescence polarization detection, luciferase reporter gene experiment (gh3), gh3 cell proliferation experiment[55]TRβ分子对接Molecular docking[49]
2.1 EDCs竞争结合ER/AR
通常,经典的核受体介导途径是性激素发挥生物学功能的重要途径。E2、T/DHT进入靶细胞后分别与雌激素核受体(nuclear estrogen receptor, nER)、雄激素核受体(nuclear androgen receptor, nAR)结合形成激素-受体复合物,然后复合物作用于靶基因上游的雌激素应答元件(estrogen response element, ERE)、雄激素应答元件(androgen response element, ARE)进而调控下游靶基因的转录。ER、AR均为配体依赖性转录因子。在没有配体存在时,受体与共抑制蛋白结合而处于抑制状态;天然配体与受体结合,使其构象发生改变,共抑制蛋白解离,共激活蛋白结合而处于激活状态[28-29]。
ER受体介导途径是EDCs发挥雌激素干扰效应的重要作用途径。目前已有很多研究表明雌激素类EDCs具有与E2相似的化学结构,可以模拟或阻断E2与哺乳动物nER的结合,激活或无法激活下游靶基因的转录,从而发挥类E2活性(ER激动剂效应)或抗E2活性(ER拮抗剂效应),并引起生殖毒性[2,6,30]。例如,邻苯二甲酸酯类[31]、双酚类化合物(如双酚A、双酚S、双酚F、双酚AF)[28,32-33]、滴滴涕及滴滴伊[34-35]、十氯酮(chlordecone)[35]等可以结合ER,发挥ER激动剂效应;而他莫昔芬[35-36]、雷洛昔芬[37]、叔丁基苯酚(tertiary butyl phenol, TBP)[38]及重金属Cd、Cu、Zn[39]等能够与E2竞争结合ER,阻断E2与ERs结合,发挥抗雌激素效应。此外,EDCs对不同的nER亚型有不同的亲和力。例如,染料木黄酮、香豆雌酚、特辛基苯酚(4-tert-octylphenol, PTOP)对ERβ的亲和力较强;药物类乙炔基雌二醇对ERα的亲和力较强[39-42]。
AR受体介导途径是EDCs发挥雄激素干扰作用的重要作用途径。一些与雄激素具有相似化学结构的EDCs,可以模拟或阻断雄激素与nAR的结合,激活或无法激活下游靶基因的转录,从而发挥类雄激素活性(AR激动剂效应)或抗雄激素活性(AR拮抗剂效应),并引起生殖毒性。例如4-羟基睾酮和4-羟基雄烯二酮[43]及BPS[27]可以结合AR,发挥AR激动效应;邻叔丁基苯酚(2-TBP)和2,4-二叔丁基苯酚(2,4-DTBP)[44]、BPA和BPF[28]及3β,4β-二羟基-5α-雄甾烷-17-酮[43]可以与T或者DHT竞争结合AR,发挥抗雄激素效应。
2.2 EDCs竞争结合TR
核受体介导的转录调节是T3发挥生物学作用的重要机制[45]。TR与维甲酸受体(retinoid X receptor, RXR)形成异源二聚体(TR-RXR);在没有配体存在时,TR-RXR与共抑制蛋白如核受体辅抑制因子(nuclear receptor corepressor, NCOR)、维甲酸和甲状腺激素受体的沉默介质(silencing mediator of retinoic acid and thyroid hormone receptor, SMRT)结合,TR-RXR处于抑制状态;T3进入靶组织细胞后,与TR-RXR结合,使得二聚体的构象发生改变,共抑制蛋白解离,共激活蛋白结合,配体、TR-RXR、共激活蛋白形成的复合物与下游靶基因DNA上的甲状腺激素应答元件(thyroid hormone response element, TRE)结合,调控下游靶基因的转录[44-48]。
TR介导途径是甲状腺干扰物(thyroid disrupting chemicals, TDCs)发挥甲状腺干扰效应的最重要作用途径。TDCs与TRβ结合后可能激活下游靶基因的转录,发挥类T3活性(TR激动剂效应),亦或无法激活下游靶基因的转录却因占据了有限的T3与TR的结合位点而发挥抗T3活性(TR拮抗剂效应)[20,25,49-51]。例如,羟基化的多氯联苯、阻燃剂磷酸三(1,3-二氯丙基)酯及其主要代谢物双(1,3-二氯-2-丙基)磷酸酯、全氟辛酸替代物氯化聚氟醚磺酸盐可以结合TRβ,发挥TR激动剂效应[49,51];而双酚S、四溴双酚A、羟基化多溴联苯(OH-BB80)和多溴联苯则与T3竞争结合TRβ,发挥拮抗作用,抑制下游基因的转录[20,25,50,52-53]。
2.3 EDCs与多种核受体的相互作用
由于直接或者间接作用,很多EDCs能够通过2种甚至2种以上受体介导途径发挥内分泌干扰作用。一方面,目前许多已知的EDCs发挥内分泌干扰作用的直接靶受体并非是单一的。例如,双酚类化合物能与ER结合,从而影响体质量和雌激素依赖性肿瘤的发生发展,也能与TR结合,进而上调多个与甲状腺细胞增殖和活性相关基因的表达,影响甲状腺功能[20,28,32-33,56-57]。TR、ER及AR被证明均是多溴联苯醚的作用靶点[57-59]。另一方面,鉴于甲状腺轴和生殖轴之间存在着复杂的交互作用,污染物对某一内分泌轴线的直接影响也可能会造成对另一轴线的间接影响。除了协同作用,2个轴线之间某些受体也存在呈竞争关系的相互作用。在CV-1细胞系中,TRα与配体结合后能够抑制ERα所介导的含有ERE的下游靶基因转录,TRβ没有类似作用;但TR却不能抑制同样受E2-ER调控的含有孕酮应答元件(progesterone response element, PRE)的下游靶基因转录[60]。在GH3细胞和JEG-3绒毛膜癌细胞中,TR与TRE结合,调控垂体糖蛋白激素α亚基的合成,E2可以抑制此过程,且体外合成的ERα可以与TRE结合[61]。这表明TR和ER之间存在竞争的可能性,且这2个核受体之间的相互作用取决于细胞类型、受体亚型、反应元件类型等因素[62]。目前尚缺乏EDCs对受体之间相互作用的影响研究。
3 EDCs与哺乳动物核受体相互作用的研究方法(Methods for studying the interaction of EDCs with mammalian nuclear receptors)
目前研究EDCs与哺乳动物核受体相互作用的主要方法包括理论计算模拟、体外结合实验、细胞增殖实验、报告基因实验等。与受体的相互作用是EDCs通过受体介导途径发挥内分泌干扰效应的前提,首先通过理论模拟、体外结合实验判断化合物能否与受体相结合。然后,通过细胞增殖实验、报告基因实验等进一步确定EDCs的具体作用方式(类天然激素活性或抗天然激素活性)。
3.1 理论计算模拟和体外结合实验研究EDCs与受体的结合情况
通过理论计算模拟可以在分子水平上预测化合物与受体之间的相互作用模式。常用的理论模拟方式有分子对接、分子动力学模拟等。其中,分子对接是依据配体与受体作用的“锁-钥原理”,模拟配体小分子与受体生物大分子相互作用的一种技术方法,对接过程中,将小分子配体放置于受体蛋白的活性残基处,寻找两者的最佳结合形态,通过软件来获得结合位点的具体信息与结合能[63]。有研究发现羟基化多溴联苯可以与TRβ结合,且占据TRβ的活性口袋,通过氢键及疏水作用形成稳定的复合物[25]。有研究将4-羟基雄烯二酮的降解产物与ERα进行分子对接,发现其与ERα在His524、Arg394和Glu353处形成氢键[43]。分子动力学模拟则通过构建近乎生理状态的受体蛋白溶剂化模型、计算机建立动态实验数据,进而达到分析受体与配体结合的自由能、配体与受体的反应过程及受体的构象变化的目的[64]。有研究通过分子动力学模拟发现BPS能与TRβ结合,导致TRβ配体结合域第11号α螺旋(Helix 11, H11) His435残基和第12号α螺旋(Helix 12, H12) Phe459残基之间的距离发生显著变化,H12相对重新定位,扰乱TRβ的构象[20]。
表面等离子共振实验及荧光偏振检测实验等体外结合实验可以用于验证化合物与受体的结合。表面等离子共振实验是将受体蛋白固定在生物传感器表面,将EDCs溶液流经生物传感器表面。受体与化合物间的结合引起生物传感器表面质量的增加,导致折射指数按比例改变。有研究用表面等离子共振实验检测到乙炔雌酚及BPA能与ER结合,推测这是它们发挥雌激素效应的机制[65]。此外,前列腺癌治疗药物卡鲁胺能与T竞争结合AR[66]。荧光偏振检测实验采用荧光标记的天然配体作为探针,将受体、荧光标记配体及不同浓度的EDCs混合,EDCs与配体竞争结合会导致体系荧光强度发生变化。有研究以荧光素标记的共激活因子SRC为探针,将探针、TR和一系列浓度BPA、BPF、BPS孵育,然后用荧光偏振法检测发现这3种双酚类化合物均可以诱导TRβ募集共激活因子[55]。
3.2 细胞增殖实验和报告基因实验确定EDCs的具体作用方式
通过细胞增殖实验、报告基因实验可以明确EDCs作为配体对受体的激动或/和拮抗活性。前者选用激素依赖型细胞,检测指标为细胞增殖率,目前最常用的细胞系为人乳腺癌细胞系MCF-7、大鼠垂体瘤细胞系GH3。MCF-7富含ER,其增殖具有雌激素依赖性[67],常作为体外模型被广泛用于检测环境化合物的类/抗E2活性或检测环境样本中是否存在雌激素类EDCs[68]。十氯酮(chlordecone)[34]、有机氯农药滴滴涕和滴滴伊[35]、双酚类[49]均通过与ERα结合,促进MCF-7的增殖,被认为是ERα激动剂。检测抗雌激素效应通常采用与类雌激素效应相似的方法,不同的是检测抗雌激素效应时需要添加E2同时暴露,通过是否能降低E2介导的效应来测试其是否具有抗雌激素效应。GH3内TR大量表达,作为一种THs依赖性生长细胞,其增殖可受TDCs与TR相互作用的影响,因此该细胞株常被用于筛选TDCs[69-71]。几种羟基化的多氯联苯在1×10-7 ~ 1×10-4 mol·L-1浓度范围内促进GH3细胞增殖[51],常用的阻燃剂磷酸三(1,3-二氯丙基)酯及其主要代谢物双(1,3-二氯-2-丙基)磷酸酯分别在20 mmol·L-1和200 mmol·L-1时促进GH3细胞增殖并调节细胞周期[49];此外,有研究发现饮用水消毒副产物碘乙酸与T3联合暴露GH3细胞可以显著降低T3激活的GH3细胞增殖,认为碘乙酸在体外具有T3拮抗活性[72]。
报告基因实验中,反应元件被剪接到报告基因上游,这些反应元件可以调控宿主细胞中报告基因表达,报告基因的表达产物通常易被检测。若化合物能够与受体结合,则会促使共激活因子结合至应答元件上,诱导下游报告基因的转录,通过测定报告基因的表达产物可以判断反应化合物与受体结合后对下游基因的调控作用。目前常用于验证EDCs受体介导途径的报告基因实验为构建重组受体基因双杂交酵母和构建荧光素酶报告基因系统。重组基因酵母选用LacZ为报告基因,通过测定其表达产物β-半乳糖苷酶的活性,即可表征化合物的类激素活性;而当内源激素与可拮抗其活性的EDCs同时存在时,内源激素诱导的β-半乳糖苷酶活性将受到抑制[73]。TBP (5×10-6~50 μmol·L-1)单独暴露重组ERα基因双杂交酵母,与溶剂对照相比,β-半乳糖苷酶活性没有显著变化;但叔丁基酚与2.5×10-4 mol·L-1 E2共同暴露时,与E2单独暴露组相比,则显著抑制了β-半乳糖苷酶活性[44]。环境相关浓度(5×10-7~50 μmol·L-1)BPS暴露重组TRβ基因双杂交酵母,与溶剂对照相比,β-半乳糖苷酶活性没有显著变化;但BPS与T3共同暴露时,与T3单独暴露组相比,BPS则显著抑制了β-半乳糖苷酶活性,且具有剂量依赖性[20]。有研究利用双杂交酵母评估羟基化多溴联苯(OH-BB80)的甲状腺干扰效应,结果显示OH-BB80 (0.005 nmol·L-1~5 μmol·L-1)在单独暴露时未出现类T3活性,但是当OH-BB80与0.5 μmol·L-1 T3共同暴露时则表现出拮抗作用,其拮抗能力呈浓度依赖性[25]。双荧光素酶报告基因实验则在细胞中用绿色荧光蛋白作为报告基因检测EDCs对靶基因表达的调控。有研究构建含有ERE的MELN细胞,发现BPA、BPF及BPS均以浓度依赖方式诱导荧光素酶表达,诱导能力BPA>BPF>BPS,且BPA和BPF可以与E2竞争结合ER[28]。有研究用人骨肉瘤细胞U2-OS构建荧光素酶报告基因体系,发现甲基三烯酮化合物能显著增强荧光信号,认为其具有雄激素效应[74]。
4 总结与展望(Summary and prospect)
采用理论计算模拟、表面等离子共振、荧光偏振、细胞增殖、报告基因等技术方法,目前已经明确了邻苯二甲酸酯类、双酚类、有机氯农药等EDCs能够竞争结合核受体(ER、AR和/或TR),以此为作用靶点,通过受体介导途径发挥内分泌干扰效应,因而产生发育毒性、生殖毒性、免疫毒性。基于目前的研究现状,我们认为未来的研究应更加注重EDCs与其他核受体的相互作用、膜受体介导途径以及体内实验与体外实验的有机结合。
4.1 EDCs对孕激素受体、维甲酸受体的相互作用仍需进一步探究
除ER、AR及TR,哺乳动物生殖轴和甲状腺轴中还存在其他核受体。例如,除了ER和AR,生殖轴中还有孕激素受体(progesterone receptor, PR)[75-76];除了TR,甲状腺轴中还有维甲酸受体(retinoic acid receptor RAR)[77-78]。这些核受体同样属于配体依赖型受体,在内分泌系统中发挥重要作用。研究证明,EDCs可以与这些核受体竞争结合发挥内分泌干扰作用。例如BPA及其衍生物四氯BPA和四溴BPA发挥PR激动剂效应[28];多溴联苯醚除了与ER、AR及TR结合发挥内分泌干扰作用外,还可以与PR结合[58-59,79]。但相较于ER、AR及TR,EDCs与PR及RAR等核受体相互作用的研究较少,需要进一步探究。
4.2 膜受体介导途径有望成为探究EDCs作用机制的新切入点
近年来,多种在细胞膜上表达的膜受体相继被发现,核受体与膜受体的同源性较低[80]。与核受体相比,尽管膜受体表达量低,但是其介导的非基因组调控途径发挥着重要的生物学功能。例如,E2、睾酮分别与位于细胞膜上的雌激素膜受体(membrane estrogen receptor, mER)、雄激素膜受体(membrane androgen receptor, mAR)结合后,诱导胞内产生多种第二信使,激活钙离子流、PKA和蛋白激酶C,从而调节其他转录因子活性,产生一系列生物学效应[81-83];T3也可以通过非基因组途径发挥作用,即不涉及nTR,而是直接由特异性整合素αv/β3受体组成的甲状腺激素膜受体(membrane thyroid hormone receptor, mTR)发挥转录调控作用[59,84-85]。最新的研究表明,EDCs可以与膜受体相互作用而发挥内分泌干扰作用[49,86-87]。例如,mTR介导途径在邻苯二甲酸二正丁酯、磷酸三(1,3-二氯丙基)酯诱导的甲状腺干扰效应中也发挥了重要作用[49,87]。BPA可以通过非基因组调控的方式对胰岛、内皮、乳腺和垂体产生快速激活效应,但是其通过何种膜受体介导这种非基因组调控效应目前尚不清楚[88]。目前对EDCs的受体介导途径研究主要集中于其竞争结合nER、nAR和nTR,膜受体介导途径或许可以成为探究EDCs作用机制的新切入点。
4.3 有必要采取体外、体内实验相结合的方式来研究EDCs的受体介导途径
除了理论模拟及体外实验,体内实验也可以用于验证EDCs干扰受体介导途径。目前,体内实验多通过受体调控的下游基因表达水平表征EDCs是否能够通过受体介导途径发挥作用。相较于操作简单、快速且干扰因素较少的体外实验,尽管体内实验中存在多种内源性因子可能对调控过程产生干扰,但却可以更真实反映地EDCs对生物体的内分泌干扰作用,减少假阴性/阳性结果。因此,有必要采取体外、体内实验相结合的方式来研究化合物的受体介导途径。例如,通过生物体暴露实验研究化合物对于下游靶基因的调控及生物学效应,然后结合体外实验验证是否是通过某些受体介导途径进行调控。这样既能够排除干扰因素,确定分子靶点,又能将分子靶点与生物学效应相结合,更好地表征化合物的内分泌干扰作用。
[1] Mattheij J A, Swarts J J, Lokerse P, et al. Effect of hypothyroidism on the pituitary-gonadal axis in the adult female rat [J]. The Journal of Endocrinology, 1995, 146(1): 87-94
[2] Bleak T C, Calaf G M. Breast and prostate glands affected by environmental substances (Review) [J]. Oncology Reports, 2021, 45(4): 20
[3] Diamanti-Kandarakis E, Bourguignon J P, Giudice L C, et al. Endocrine-disrupting chemicals: An Endocrine Society scientific statement [J]. Endocrine Reviews, 2009, 30(4): 293-342
[4] Frye C A, Bo E, Calamandrei G, et al. Endocrine disrupters: A review of some sources, effects, and mechanisms of actions on behaviour and neuroendocrine systems [J]. Journal of Neuroendocrinology, 2012, 24(1): 144-159
[5] Quagliariello V, Rossetti S, Cavaliere C, et al. Correction: Metabolic syndrome, endocrine disruptors and prostate cancer associations: Biochemical and pathophysiological evidences [J]. Oncotarget, 2017, 8(37): 62816
[6] Patrick S M, Bornman M S, Joubert A M, et al. Effects of environmental endocrine disruptors, including insecticides used for malaria vector control on reproductive parameters of male rats [J]. Reproductive Toxicology, 2016, 61: 19-27
[7] Rattan S, Zhou C Q, Chiang C, et al. Exposure to endocrine disruptors during adulthood: Consequences for female fertility [J]. The Journal of Endocrinology, 2017, 233(3): R109-R129
[8] Zoeller R T, Brown T R, Doan L L, et al. Endocrine-disrupting chemicals and public health protection: A statement of principles from The Endocrine Society [J]. Endocrinology, 2012, 153(9): 4097-4110
[9] Bokobza E, Hinault C, Tiroille V, et al. The adipose tissue at the crosstalk between EDCs and cancer development [J]. Frontiers in Endocrinology, 2021, 12: 691658
[10] Jeon B K, Jang Y, Lee E M, et al. A systematic approach to metabolic characterization of thyroid-disrupting chemicals and their in vitro biotransformants based on prediction-assisted metabolomic analysis [J]. Journal of Chromatography A, 2021, 1649: 462222
[11] 刘晓晨, 刘璟. 环境内分泌干扰物影响垂体促性腺激素的研究进展[J]. 生态毒理学报, 2022, 17(2): 1-19
Liu X C, Liu J. Influences of endocrine-disrupting chemicals on pituitary gonadotropins: A review [J]. Asian Journal of Ecotoxicology, 2022, 17(2): 1-19 (in Chinese)
[12] Rubin B S, Murray M K, Damassa D A, et al. Perinatal exposure to low doses of bisphenol A affects body weight, patterns of estrous cyclicity, and plasma LH levels [J]. Environmental Health Perspectives, 2001, 109(7): 675-680
[13] Hill C E, Sapouckey S A, Suvorov A, et al. Developmental exposures to bisphenol S, a BPA replacement, alter estrogen-responsiveness of the female reproductive tract: A pilot study [J]. Cogent Medicine, 2017, 4(1): 1317690
[14] Pogrmic K, Fa S, Dakic V, et al. Atrazine oral exposure of peripubertal male rats downregulates steroidogenesis gene expression in Leydig cells [J]. Toxicological Sciences: An Official Journal of the Society of Toxicology, 2009, 111(1): 189-197
[15] Munier M, Grouleff J, Gourdin L, et al. In vitro effects of the endocrine disruptor p,p’-DDT on human follitropin receptor [J]. Environmental Health Perspectives, 2016, 124(7): 991-999
[16] Moody S, Goh H, Bielanowicz A, et al. Prepubertal mouse testis growth and maturation and androgen production are acutely sensitive to di-n-butyl phthalate [J]. Endocrinology, 2013, 154(9): 3460-3475
[17] Lichtensteiger W, Ceccatelli R, Faass O, et al. Effect of polybrominated diphenylether and PCB on the development of the brain-gonadal axis and gene expression in rats [J]. Organohalogen Compounds, 2003, 61: 84-87
[18] Meeker J D, Hauser R. Exposure to polychlorinated biphenyls (PCBs) and male reproduction [J]. Systems Biology in Reproductive Medicine, 2010, 56(2): 122-131
[19] Krishnamoorthy G, Venkataraman P, Arunkumar A, et al. Ameliorative effect of vitamins (alpha-tocopherol and ascorbic acid) on PCB (Aroclor 1254) induced oxidative stress in rat epididymal sperm [J]. Reproductive Toxicology, 2007, 23(2): 239-245
[20] Lu L P, Zhan T J, Ma M, et al. Thyroid disruption by bisphenol S analogues via thyroid hormone receptor β: in vitro, in vivo, and molecular dynamics simulation study [J]. Environmental Science &Technology, 2018, 52(11): 6617-6625
[21] Sharan S, Nikhil K, Roy P. Disruption of thyroid hormone functions by low dose exposure of tributyltin: An in vitro and in vivo approach [J]. General and Comparative Endocrinology, 2014, 206: 155-165
[22] Ahmed R G. Maternal bisphenol A alters fetal endocrine system: Thyroid adipokine dysfunction [J]. Food and Chemical Toxicology, 2016, 95: 168-174
[23] Hammouda F, Messaoudi I, El Hani J, et al. Reversal of cadmium-induced thyroid dysfunction by selenium, zinc, or their combination in rat [J]. Biological Trace Element Research, 2008, 126(1-3): 194-203
[24] Ghisari M, Bonefeld-Jorgensen E C. Effects of plasticizers and their mixtures on estrogen receptor and thyroid hormone functions [J]. Toxicology Letters, 2009, 189(1): 67-77
[25] Zhang X F, Cui S X, Pan L M, et al. The molecular mechanism of the antagonistic activity of hydroxylated polybrominated biphenyl (OH-BB80) toward thyroid receptor Β [J]. The Science of the Total Environment, 2019, 697: 134040
[26] Kim M J, Park Y J. Bisphenols and thyroid hormone [J]. Endocrinology and Metabolism, 2019, 34(4): 340-348
[27] Sheng Z G, Tang Y, Liu Y X, et al. Low concentrations of bisphenol A suppress thyroid hormone receptor transcription through a nongenomic mechanism [J]. Toxicology and Applied Pharmacology, 2012, 259(1): 133-142
[28] Molina-Molina J M, Amaya E, Grimaldi M, et al. In vitro study on the agonistic and antagonistic activities of bisphenol-S and other bispheno-A congeners and derivatives via nuclear receptors [J]. Toxicology and Applied Pharmacology, 2013, 272(1): 127-136
[29] McEwan I J, Brinkmann A O. Androgen Physiology: Receptor and Metabolic Disorders [M]. South Dartmouth: MDText.com, Inc., 2000
[30] Cariati F, D’Uonno N, Borrillo F, et al. Bisphenol A: An emerging threat to male fertility [J]. Reproductive Biology and Endocrinology, 2019, 17(1): 6
[31] 席令仪, 潘志辉, 段晨晖, 等. 几种典型邻苯二甲酸酯类增塑剂对雌激素受体的干扰效应研究[C]// 中国毒理学会计算毒理专业委员. 第四次全国计算毒理学学术会议暨国家自然科学基金委员会化学科学部学科战略研讨会论文集, 延安, 2021-07
[32] Cao H M, Wang F B, Liang Y, et al. Experimental and computational insights on the recognition mechanism between the estrogen receptor α with bisphenol compounds [J]. Archives of Toxicology, 2017, 91(12): 3897-3912
[33] Mesnage R, Phedonos A, Arno M, et al. Editor’s highlight: Transcriptome profiling reveals bisphenol A alternatives activate estrogen receptor alpha in human breast cancer cells [J]. Toxicological Sciences, 2017, 158(2): 431-443
[34] Okubo T, Yokoyama Y, Kano K, et al. Estimation of estrogenic and antiestrogenic activities of selected pesticides by MCF-7 cell proliferation assay [J]. Archives of Environmental Contamination and Toxicology, 2004, 46(4): 445-453
[35] Andersen H R, Andersson A M, Arnold S F, et al. Comparison of short-termestrogenicity tests for identification of hormone-disrupting chemicals [J]. Environmental Health Perspectives, 1999, 107(Suppl 1): 89-108
[36] 王建逵, 李明, 杨晓娟, 等. 他莫昔芬对乳腺癌患者的雌激素受体α36的增强转移作用[J]. 中国临床药理学杂志, 2018, 34(9): 1042-1044
Wang J K, Li M, Yang X J, et al. Enhance transfer function of tamoxifen on the estrogen receptor α 36 in the breast cancer patients [J]. The Chinese Journal of Clinical Pharmacology, 2018, 34(9): 1042-1044 (in Chinese)
[37] 王佩, 李玉珍. 雷洛昔芬——选择性雌激素受体调节剂[J]. 药物不良反应杂志, 2004, 6(5): 320-322
Wang P, Li Y Z. Raloxifene: A selective estrogen receptor mediator [J]. Adverse Drug Reactions Journal, 2004, 6(5): 320-322 (in Chinese)
[38] Kitamura S, Jinno N, Ohta S, et al. Thyroid hormonal activity of the flame retardants tetrabromobisphenol A and tetrachlorobisphenol A [J]. Biochemical and Biophysical Research Communications, 2002, 293(1): 554-559
[39] 季晓亚, 李娜, 袁圣武, 等. 环境雌激素生物效应的作用机制研究进展[J]. 生态毒理学报, 2017, 12(1): 38-51
Ji X Y, Li N, Yuan S W, et al. Research progress in the mechanisms for biological effects of environmental estrogens [J]. Asian Journal of Ecotoxicology, 2017, 12(1): 38-51 (in Chinese)
[40] 黄苑, 苏晓鸥, 王瑞国, 等. 多氯联苯羟基化代谢物及其雌激素效应研究进展[J]. 生态毒理学报, 2018, 13(5): 58-68
Huang Y, Su X O, Wang R G, et al. Advances on hydroxylated polychlorinated biphenyls metabolites and the estrogenic effects [J]. Asian Journal of Ecotoxicology, 2018, 13(5): 58-68 (in Chinese)
[41] Escande A, Pillon A, Servant N, et al. Evaluation of ligand selectivity using reporter cell lines stably expressing estrogen receptor alpha or beta [J]. Biochemical Pharmacology, 2006, 71(10): 1459-1469
[42] 朱婧涵, 薛峤, 张爱茜. 对特辛基苯酚干扰雌激素受体作用的分子基础及其对ERβ亚型选择性结合的理论研究[J]. 生态毒理学报, 2016, 11(2): 194-200
Zhu J H, Xue Q, Zhang A Q. Structural basis and molecular mechanism for selective binding of 4-tertoctylphenol to estrogen receptor [J]. Asian Journal of Ecotoxicology, 2016, 11(2): 194-200 (in Chinese)
[43] Keiler A M, Zierau O, Wolf S, et al. Androgen- and estrogen-receptor mediated activities of 4-hydroxytestosterone, 4-hydroxyandrostenedione and their human metabolites in yeast based assays [J]. Toxicology Letters, 2018, 292: 39-45
[44] Wang J Y, Wang J P, Liu J S, et al. The evaluation of endocrine disrupting effects of tert-butylphenols towards estrogenic receptor α, androgen receptor and thyroid hormone receptor β and aquatic toxicities towards freshwater organisms [J]. Environmental Pollution, 2018, 240: 396-402
[45] Ya ar P, Ayaz G, User S D, et al. Molecular mechanism of estrogen-estrogen receptor signaling [J]. Reproductive Medicine and Biology, 2017, 16(1): 4-20
ar P, Ayaz G, User S D, et al. Molecular mechanism of estrogen-estrogen receptor signaling [J]. Reproductive Medicine and Biology, 2017, 16(1): 4-20
[46] Shibusawa N, Hollenberg A N, Wondisford F E. Thyroid hormone receptor DNA binding is required for both positive and negative gene regulation [J]. The Journal of Biological Chemistry, 2003, 278(2): 732-738
[47] Wu Y F, Koenig R J. Gene regulation by thyroid hormone [J]. Trends in Endocrinology &Metabolism, 2000, 11(6): 207-211
[48] Yen P M. Physiological and molecular basis of thyroid hormone action [J]. Physiological Reviews, 2001, 81(3): 1097-1142
[49] Yu C, Wang C, Lu Z B, et al. The endocrine-disrupting potential of four chlorophenols by in vitro and in silico assay [J]. Chemosphere, 2019, 218: 941-947
[50] Yang J, Chan K M. Evaluation of the toxic effects of brominated compounds (BDE-47, 99, 209, TBBPA) and bisphenol A (BPA) using a zebrafish liver cell line, ZFL [J]. Aquatic Toxicology, 2015, 159: 138-147
[51] Kitamura S, Jinno N, Ohta S, et al. Thyroid hormonal activity of the flame retardants tetrabromobisphenol A and tetrachlorobisphenol A [J]. Biochemical and Biophysical Research Communications, 2002, 293(1): 554-559
[52] 张婧. 双酚A对F344大鼠甲状腺组织雌激素受体α表达的影响[D]. 济南: 山东大学, 2017: 10-26
Zhang J. The effect of bisphenol A on expression of estrogen receptor α in thyroids of F344 rats [D]. Ji’nan: Shandong University, 2016: 10-26 (in Chinese)
[53] 胡伟婷, 关海霞, 滕卫平. 环境内分泌干扰物对甲状腺影响[J]. 中国公共卫生, 2013, 29(2): 306-309
[54] Li F, Xie Q, Li X H, et al. Hormone activity of hydroxylated polybrominated diphenyl ethers on human thyroid receptor-beta: in vitro and in silico investigations [J]. Environmental Health Perspectives, 2010, 118(5): 602-606
[55] Zhang Y F, Ren X M, Li Y Y, et al. Bisphenol A alternatives bisphenol S and bisphenol F interfere with thyroid hormone signaling pathway in vitro and in vivo [J]. Environmental Pollution, 2018, 237: 1072-1079
[56] Cimmino I, Fiory F, Perruolo G, et al. Potential mechanisms of bisphenol A (BPA) contributing to human disease [J]. International Journal of Molecular Sciences, 2020, 21(16): 5761
[57] Gorini F, Bustaffa E, Coi A, et al. Bisphenols as environmental triggers of thyroid dysfunction: Clues and evidence [J]. International Journal of Environmental Research and Public Health, 2020, 17(8): 2654
[58] Hamers T, Kamstra J H, Sonneveld E, et al. In vitro profiling of the endocrine-disrupting potency of brominated flame retardants [J]. Toxicological Sciences: An Official Journal of the Society of Toxicology, 2006, 92(1): 157-173
[59] Hamers T, Kamstra J H, Sonneveld E, et al. Biotransformation of brominated flame retardants into potentially endocrine-disrupting metabolites, with special attention to 2,2’,4,4’-tetrabromodiphenyl ether (BDE-47) [J]. Molecular Nutrition &Food Research, 2008, 52(2): 284-298
[60] Scott R E, Wu-Peng X S, Yen P M, et al. Interactions of estrogen- and thyroid hormone receptors on a progesterone receptor estrogen response element (ERE) sequence: A comparison with the vitellogenin A2 consensus ERE [J]. Molecular Endocrinology, 1997, 11(11): 1581-1592
[61] Yarwood N J, Gurr J A, Sheppard M C, et al. Estradiol modulates thyroid hormone regulation of the human glycoprotein hormone alpha subunit gene [J]. The Journal of Biological Chemistry, 1993, 268(29): 21984-21989
[62] Zsarnovszky A, Kiss D, Jocsak G, et al. Thyroid hormone- and estrogen receptor interactions with natural ligands and endocrine disruptors in the cerebellum [J]. Frontiers in Neuroendocrinology, 2018, 48: 23-36
[63] Pinzi, Rastelli G. Molecular docking: Shifting paradigms in drug discovery [J]. International Journal of Molecular Sciences, 2019, 20(18): 4331
[64] 门通. 新型冠状病毒主蛋白酶与其潜在抑制剂相互作用的分子动力学模拟[D]. 长春: 吉林大学, 2021: 12-42
Men T. Molecular dynamics simulation of the interaction between the novel coronavirus main protease and its potential inhibitors [D]. Changchun: Jilin University, 2021: 12-42 (in Chinese)
[65] Usami M, Mitsunaga K, Ohno Y. Estrogen receptor binding assay of chemicals with a surface plasmon resonance biosensor [J]. The Journal of Steroid Biochemistry and Molecular Biology, 2002, 81(1): 47-55
[66] Fortugno C, Varchi G, Guerrini A, et al. Optical biosensor analysis in studying new synthesized bicalutamide analogs binding to androgen receptor [J]. Journal of Pharmaceutical and Biomedical Analysis, 2014, 95: 151-157
[67] Combes R D. Endocrine disruptors: A critical review of in vitro and in vivo testing strategies for assessing their toxic hazard to humans [J]. Alternatives to Laboratory Animals, 2000, 28(1): 81-118
[68] Tanji M, Katz B H, Spink B C, et al. Growth inhibition of MCF-7 cells by estrogen is dependent upon a serum factor [J]. Anticancer Research, 2000, 20(4): 2779-2783
[69] Ghisari M, Bonefeld-Jorgensen E C. Impact of environmental chemicals on the thyroid hormone function in pituitary rat GH3 cells [J]. Molecular and Cellular Endocrinology, 2005, 244(1-2): 31-41
[70] Gutleb A C, Meerts I A, Bergsma J H, et al. T-Screen as a tool to identify thyroid hormone receptor active compounds [J]. Environmental Toxicology and Pharmacology, 2005, 19(2): 231-238
[71] Kim S, Jung J, Lee I, et al. Thyroid disruption by triphenyl phosphate, an organophosphate flame retardant, in zebrafish (Danio rerio) embryos/larvae, and in GH3 and FRTL-5 cell lines [J]. Aquatic Toxicology, 2015, 160: 188-196
[72] Xia Y, Mo Y, Yang Q Y, et al. Iodoacetic acid disrupting the thyroid endocrine system in vitro and in vivo [J]. Environmental Science &Technology, 2018, 52(13): 7545-7552
[73] 李剑, 任姝娟, 马梅, 等. 改进型重组基因酵母TR-GRIP1检测化合物甲状腺激素干扰活性[J]. 环境科学研究, 2011, 24(10): 1172-1177
Li J, Ren S J, Ma M, et al. Use of modified recombinant gene yeast TR-GRIP1 to screen chemicals for thyroid disrupting activity [J]. Research of Environmental Sciences, 2011, 24(10): 1172-1177 (in Chinese)
[74] Sonneveld E, Riteco J A C, Jansen H J, et al. Comparison of in vitro and in vivo screening models for androgenic and estrogenic activities [J]. Toxicological Sciences, 2006, 89(1): 173-187
[75] Grimm S L, Hartig S M, Edwards D P. Progesterone receptor signaling mechanisms [J]. Journal of Molecular Biology, 2016, 428(19): 3831-3849
[76] Rowan B G, O’Malley B W. Progesterone receptor coactivators [J]. Steroids, 2000, 65(10-11): 545-549
[77] Burris T P, Nawaz Z, Tsai M J, et al. A nuclear hormone receptor-associated protein that inhibits transactivation by the thyroid hormone and retinoic acid receptors [J]. Proceedings of the National Academy of Sciences of the United States of America, 1995, 92(21): 9525-9529
[78] Alvarez S, Bourguet W, Gronemeyer H, et al. Retinoic acid receptor modulators: A perspective on recent advances and promises [J]. Expert Opinion on Therapeutic Patents, 2011, 21(1): 55-63
[79] Ren X M, Guo L H, Gao Y, et al. Hydroxylated polybrominated diphenyl ethers exhibit different activities on thyroid hormone receptors depending on their degree of bromination [J]. Toxicology and Applied Pharmacology, 2013, 268(3): 256-263
[80] Fuentes N, Silveyra P. Estrogen receptor signaling mechanisms [J]. Advances in Protein Chemistry and Structural Biology, 2019, 116: 135-170
[81] Hammes S R, Levin E R. Extranuclear steroid receptors: Nature and actions [J]. Endocrine Reviews, 2007, 28(7): 726-741
[82] Thomas P. Rapid steroid hormone actions initiated at the cell surface and the receptors that mediate them with an emphasis on recent progress in fish models [J]. General and Comparative Endocrinology, 2012, 175(3): 367-383
[83] Tokarz J, Möller G, Hrabě de Angelis M, et al. Steroids in teleost fishes: A functional point of view [J]. Steroids, 2015, 103: 123-144
[84] Davis P J, Zhou M, Davis F B, et al. Mini-review: Cell surface receptor for thyroid hormone and nongenomic regulation of ion fluxes in excitable cells [J]. Physiology &Behavior, 2010, 99(2): 237-239
[85] Hammes S R, Davis P J. Overlapping nongenomic and genomic actions of thyroid hormone and steroids [J]. Best Practice &Research Clinical Endocrinology &Metabolism, 2015, 29(4): 581-593
[86] Nadal A, Fuentes E, Ripoll C, et al. Extranuclear-initiated estrogenic actions of endocrine disrupting chemicals: Is there toxicology beyond Paracelsus? [J]. The Journal of Steroid Biochemistry and Molecular Biology, 2018, 176: 16-22
[87] Kong X T, Sun H Y, Pan P C, et al. Importance of protein flexibility in molecular recognition: A case study on Type-I1/2 inhibitors of ALK [J]. Physical Chemistry Chemical Physics, 2018, 20(7): 4851-4863
[88] Alonso-Magdalena P, Laribi O, Ropero A B, et al. Low doses of bisphenol A and diethylstilbestrol impair Ca2+ signals in pancreatic alpha-cells through a nonclassical membrane estrogen receptor within intact islets of Langerhans [J]. Environmental Health Perspectives, 2005, 113(8): 969-977